As many people reading this will no doubt already be aware, Tara Shennan and I have submitted a BACP AGM resolution asking BACP to end its association with the SCoPEd project and that any future move towards developing competency framework must be undertaken with full membership consultation from the outset.
So what has led to this unprecedented action? The more I have dealt with the BACP, the more frustrated I have become by their seemingly pre-rehearsed lines and steadfast refusal to entertain the idea that SCoPEd is in fact not in the best interests of clients, therapists, the BACP or the profession. There is another Q&A planned for BACP members, and I fully expect to hear the same lines we have heard over and over again: ‘entry points’, ‘evidence-based’, ‘creating opportunities’, ‘we got the language wrong’, ‘we’re listening’ and so on, without directly addressing any of the problems that have been raised with these lines, such as the disprovability of the ‘evidence’, the fact that ‘accredited therapist’ is not an entry point, the lack of evidence that this will create jobs, and so on.
I haven’t taken the decision to submit the resolution lightly; I am aware that the profession I love is at an extremely difficult point in its history, and that the result of this resolution represents a crossroads for BACP, its members, clients and the wider profession. It is rather surreal to find myself so centrally involved in this pivotal moment. But I can see the crossroads ahead, and I can see the path that the BACP are aiming for. It is a path which forces psychotherapists to accept an increasing alignment with the medical model, that casts counselling as psychotherapy’s poor relation and dismisses counsellors as incapable of some of the most basic therapeutic skills. It is a path of IAPT, of elitism, of hierarchy, power and endless volunteering. It is not a path I am willing to let therapy go down.
The first round of resolution voting opens on 19th August and closes 10th September. If you are a BACP member, you will receive an email from BACP (or someone from BACP, or mi vote) providing you with a unique voting link. This vote will decide whether or not the resolution will get through to an AGM vote. If you are a BACP member (including student member) we really, really, need your vote on this because the bar has been set very high – we need 5% of the entire BACP membership to vote for our resolution. That is approximately 2500 members. Unlike BACP, we do not have means to contact all of the members to make them aware of the importance of this vote. So please spread the word, amongst colleagues, friends, fellow students, at networking meetings, conferences, on social media, please keep talking #SCoPEd and help us overcome the massive imbalance of power we are facing in this campaign.
The second round of voting is the actual AGM vote. Again you will receive an email from the BACP or mi vote with a unique link to cast your vote. Online voting for the AGM opens 1st October and closes 4th November. If you are intending to attend the AGM, you may vote in person instead. Rather than needing a particular percentage, for this round we need a simple majority. This means we need to get more votes in favour of the resolution than there are votes against. Again, we need everyone’s support and vote in this round. BACP will be doing everything they can to encourage people to vote against the resolution, so it is hugely important to make your voice heard in this, the deciding vote.
If we are successful in securing a majority in the AGM round, BACP will be legally bound to implement the resolution and discontinue their association with the project. This would be a fantastic result for therapists, clients and for counselling and psychotherapy. It will also be an important message for the membership bodies to hear – the bodies must not lose sight of their responsibility to members, and we will make our voices heard.
For those who haven’t seen it (and even for those who have!) here is the wording of our resolution:
Summary
It is proposed that the BACP discontinue their association with the SCoPEd project, which portrays counsellors as less competent than psychotherapists and questions their capacity for independent judgement. Furthermore, we propose that any future move towards developing a competency framework must be undertaken with member-consultation from the outset.
Explanatory Statement
We propose that BACP discontinue their association with the controversial SCoPEd project, and that any future move to develop a competency framework should be undertaken with member-consultation from the outset.
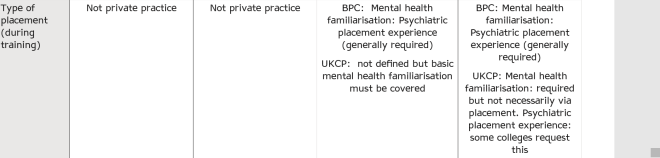
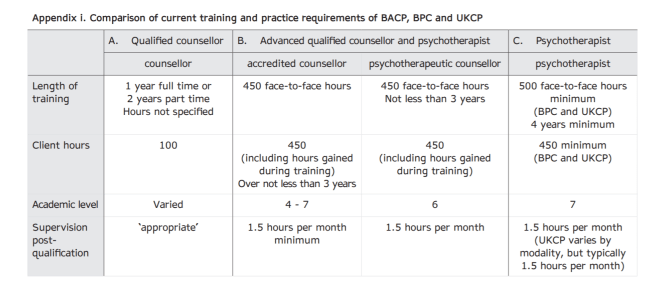
Communication with members has been poor, and many members are unhappy with the way the research has been conducted. The joint project between BACP, UKCP and BPC was developed without any initial member-consultation. The majority of the expert reference group are psychoanalyst/psychodynamic therapists, and several modalities are unrepresented, including person-centred therapy.
The tiered system presented in the project favours trainings associated with two of the bodies involved with the project – UKCP and BPC. While the authors of this resolution do not suggest any impropriety from researchers, we suggest the absence of declarations of potential conflicts of interest is a serious ethical limitation of the research.
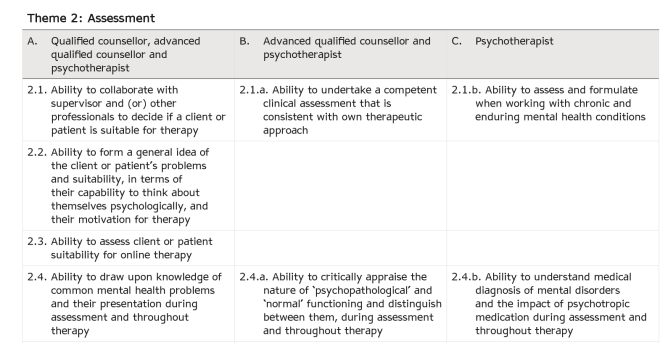
The SCoPEd framework places counsellors and psychotherapists on a competency continuum which deskills counsellors, and is not reflective of the ways in which members work in reality.
Claims that SCoPEd will provide clarity for clients, therapists and other stakeholders are called into question by members who report feeling confused by the project. The SCoPEd team have said the terms ‘counsellor’ and ‘psychotherapist’ are not titles, while presumably the evidence they draw upon in the research would use these terms as titles.
BACP have said that the tiers are ‘entry points’, yet ‘Advanced Counsellor’ is only attainable for the vast majority of members through accreditation or equivalent post-qualification experience, which is not an entry point. Facebook chats and Therapy Today articles appear to have only obfuscated further. Members are concerned about what SCoPEd means for the future, because the BACP are not providing clarity about this.
Additionally, concerns have been expressed about the use of medicalised language in the framework, which does not reflect the diversity of modalities and therapeutic approaches amongst members. This comes as movement to challenge the medicalisation of distress gains traction in the field (See: Power Threat Meaning Framework, Johnstone and Boyle, 2018).
If this resolution is successful, the BACP will discontinue its association with the SCoPEd project. This will mean that the tiered framework will not be implemented for BACP members, and the BACP will not spend members’ fees and resources on its further development or implementation. The authors of this resolution propose that this is in the interests of the organisation, its members and clients.
If this resolution is unsuccessful, we do not know what this will mean for the future of the BACP or the profession. At the very least, it is likely that courses leading to UKCP and BPC membership will be seen as preferable from the perspective of new students, employers and perhaps even insurers, since SCoPEd declares therapists entering the profession with those qualifications to possess higher competencies around assessment, ethics, ruptures, unconscious processes and more. The authors suggest that these propositions are damaging, do not reflect the realities of training and practice, and are based on flawed research.
And for anyone who got the reference in the title, or didn’t but is curious anyway, here’s a bonus bit of listening: Talkin’ ‘Bout a Revolution